Let's talk about salpingectomy
70 to 80% of ovarian cancer actually originates from the fallopian tube. That’s why removing both fallopian tubes (bilateral salpingectomy) can substantially decrease the risk of ovarian cancer. Incorporating this into other planned abdominal surgeries may be the best opportunity to prevent ovarian cancer.

Removing both fallopian tubes can help reduce ovarian cancer risk
There is no effective way to screen for or diagnose ovarian cancer in its earliest forms. A recent study of hundreds of thousands of women showed that screening with ultrasounds and blood testing did not save as many lives as hoped. In fact, ineffective screening leads to false reassurance (via false negative results).
The good news!
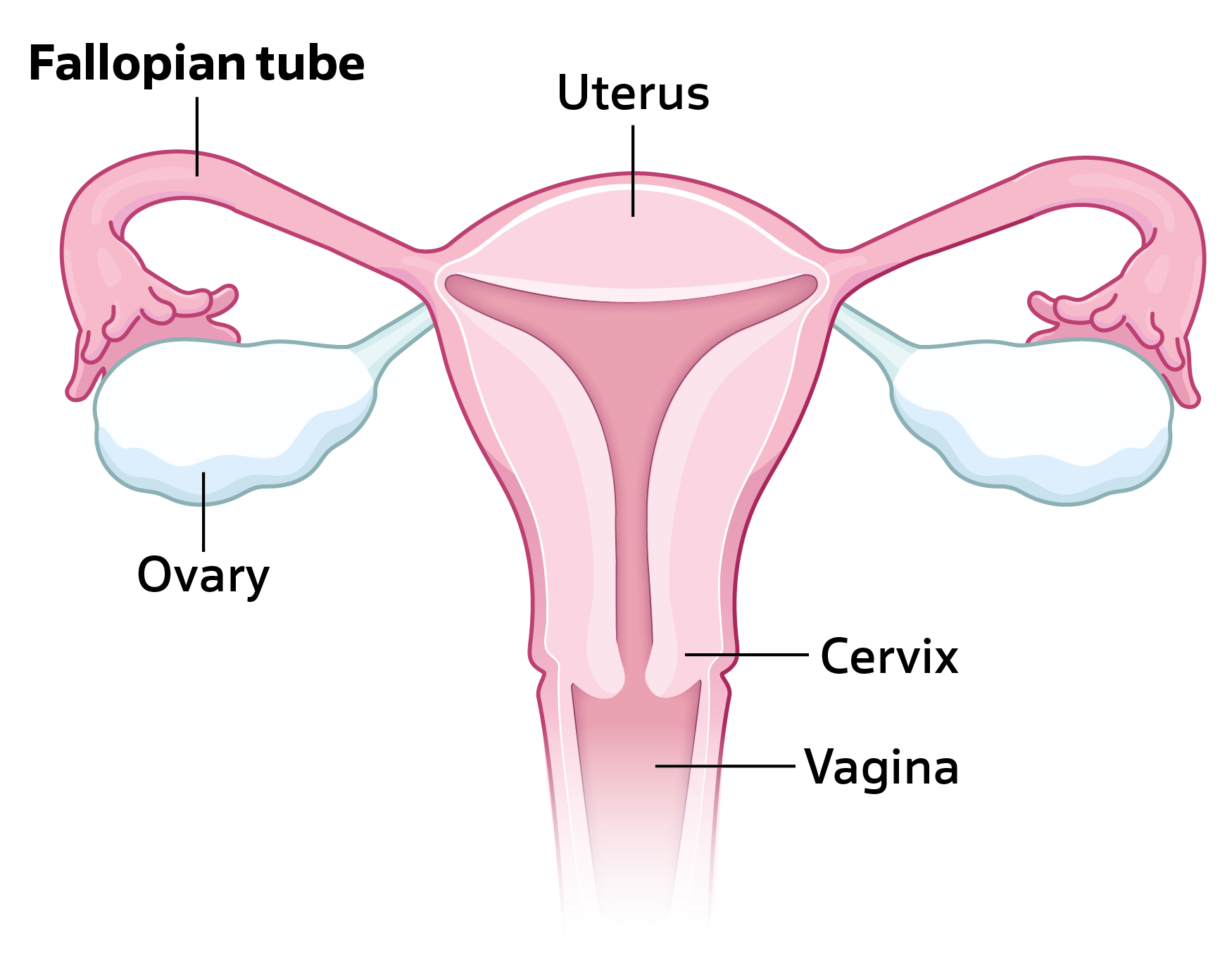
The recent discovery that most ovarian cancer begins in the fallopian tubes has led to a new opportunity. The newest opportunity is bilateral salpingectomy. Salpingectomy is the removal of the fallopian tubes. It can be offered to patients at the time of hysterectomy, instead of tubal ligation and during other abdominal surgeries. The ovaries are left in place during a salpingectomy.
Bilateral salpingectomy—a promising intervention for reducing ovarian cancer risk
Large studies have found that removing both fallopian tubes (called bilateral salpingectomy) can lower the risk of ovarian cancer by more than half. In particular, research from Canada shows that it can help prevent most cases of high-grade serous cancer—the most common and deadly type of ovarian cancer.
It may also lower the risk of other serious types like endometrioid and clear cell ovarian cancer.
Bilateral salpingectomy does not reduce the risk of rare types like germ cell or sex cord-stromal tumors. Fortunately, these usually have better outcomes.
Research consistently shows that bilateral salpingectomy does not increase the risk of surgical complications, such as infection or hospital readmission (the need to come back to the hospital for a problem once home after surgery).
Bilateral salpingectomy does not negatively affect ovarian function, fertility outcomes, or cause earlier menopause in premenopausal women. Clinical trials and large observational studies confirm that bilateral salpingectomy can be safely performed during other routine abdominal or gynecologic surgeries.
According to a study looking at physician visits for menopause and hormone replacement therapy:
- There was no indication that salpingectomy causes menopause to begin earlier.
This is because:- the fallopian tubes do not make hormones
- the ovaries make hormones and are left in place
How many patients will this impact:
Thousands of ovarian cancers could be eliminated every year in the U.S. if everyone who wanted permanent birth control could choose:
- to have their fallopian tubes completely removed (salpingectomy) instead of just tying them
- to have their fallopian tubes removed during a hysterectomy or another planned abdominal surgery
Long-term use (typically five or more years) of hormonal contraception, like birth control pills, can lower the risk of ovarian cancer by 40–50%. This is likely because the number of ovulations over a lifetime are reduced.
Tubal ligation slightly reduces the risk of some ovarian cancers (like endometrioid and clear cell), but not the most common and deadly type—serous ovarian cancer.
To see how these options and other options compare to salpingectomy for lowering ovarian cancer risk, check out ‘Know Your Contraception Options’ in the Resources tab.
Ovarian cancer is a misnomer
For many years, all these different types of cancer were thought to start in the ovary. Some, like low-grade serous cancers, germ cell tumors, and stromal tumors, do start in the ovary. But research over the last 20 years has revealed that most other types actually begin in or are linked to the fallopian tube. One rare type—called mucinous cancer—is still not fully understood and may come from somewhere else in the body, like the digestive tract.
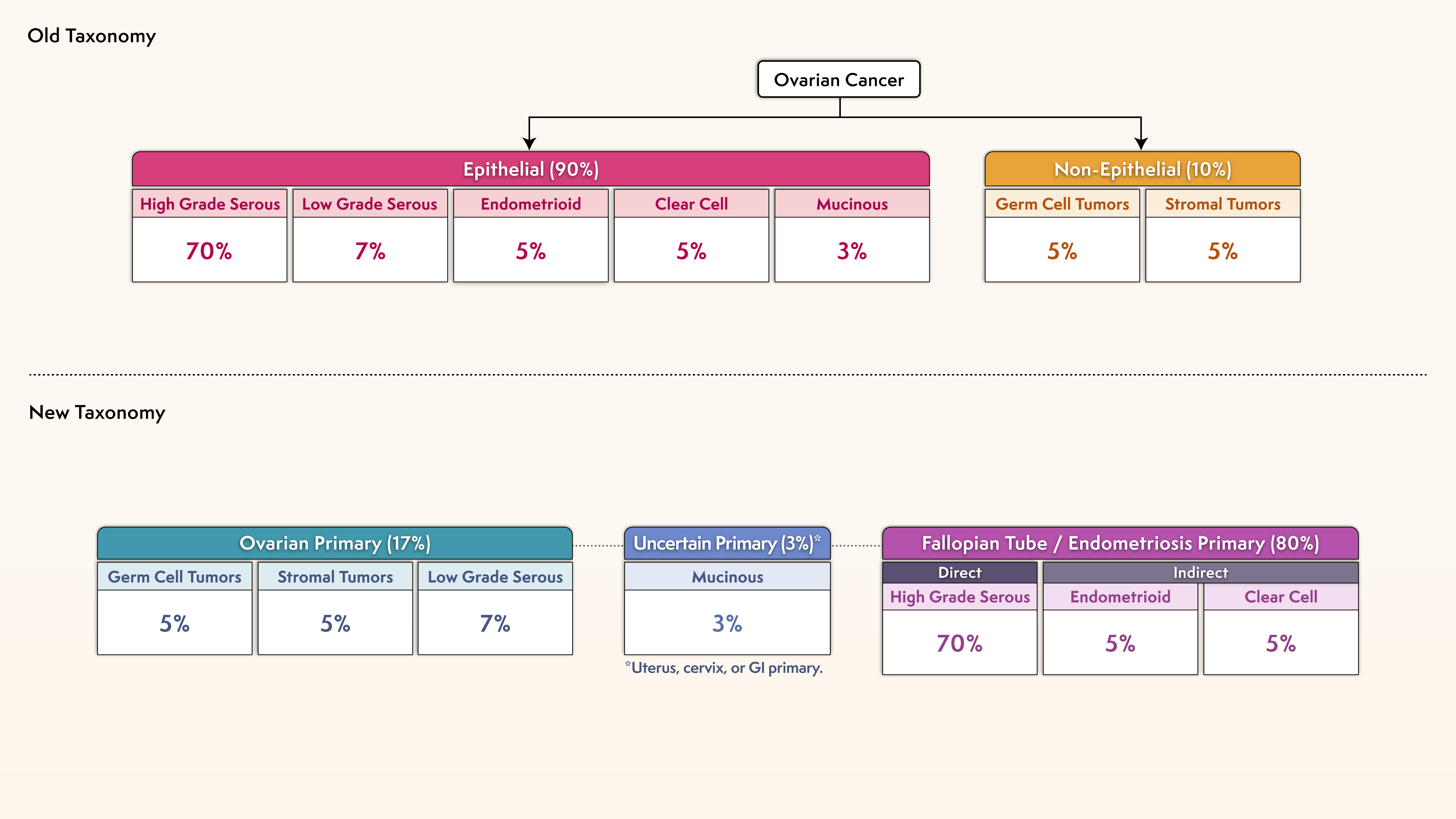
High-grade serous carcinoma is the most common type of ovarian cancer
Ovarian carcinoma is a highly heterogenous group of diseases, including different histological subtypes. Among them, high-grade serous carcinoma (HGSC) accounts for 70% of ovarian cancer. And it is the most lethal.
Stage at Diagnosis: HGSC
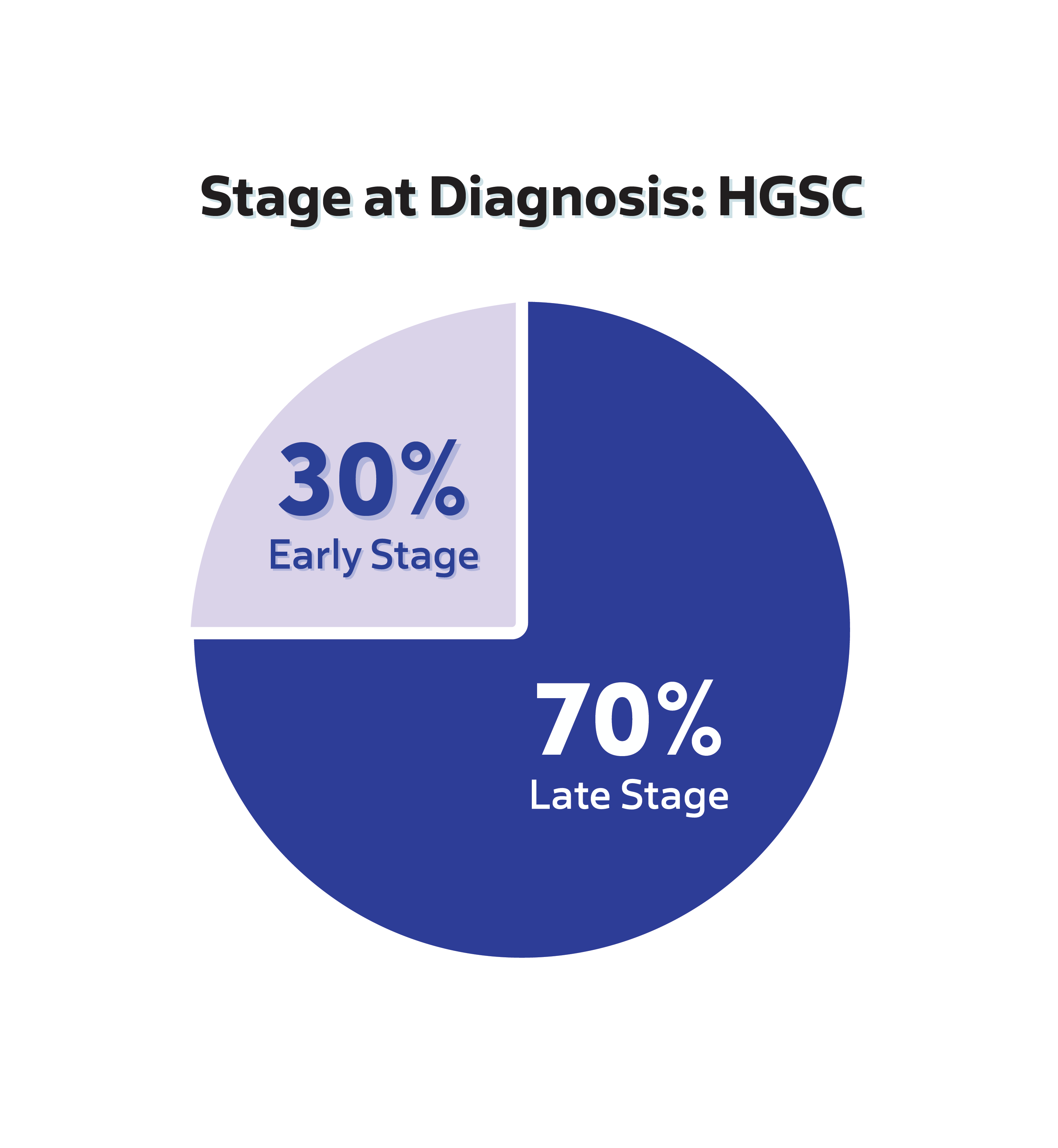
70% of HGSC cases are diagnosed at a late stage
HGSC Diagnosis Stage
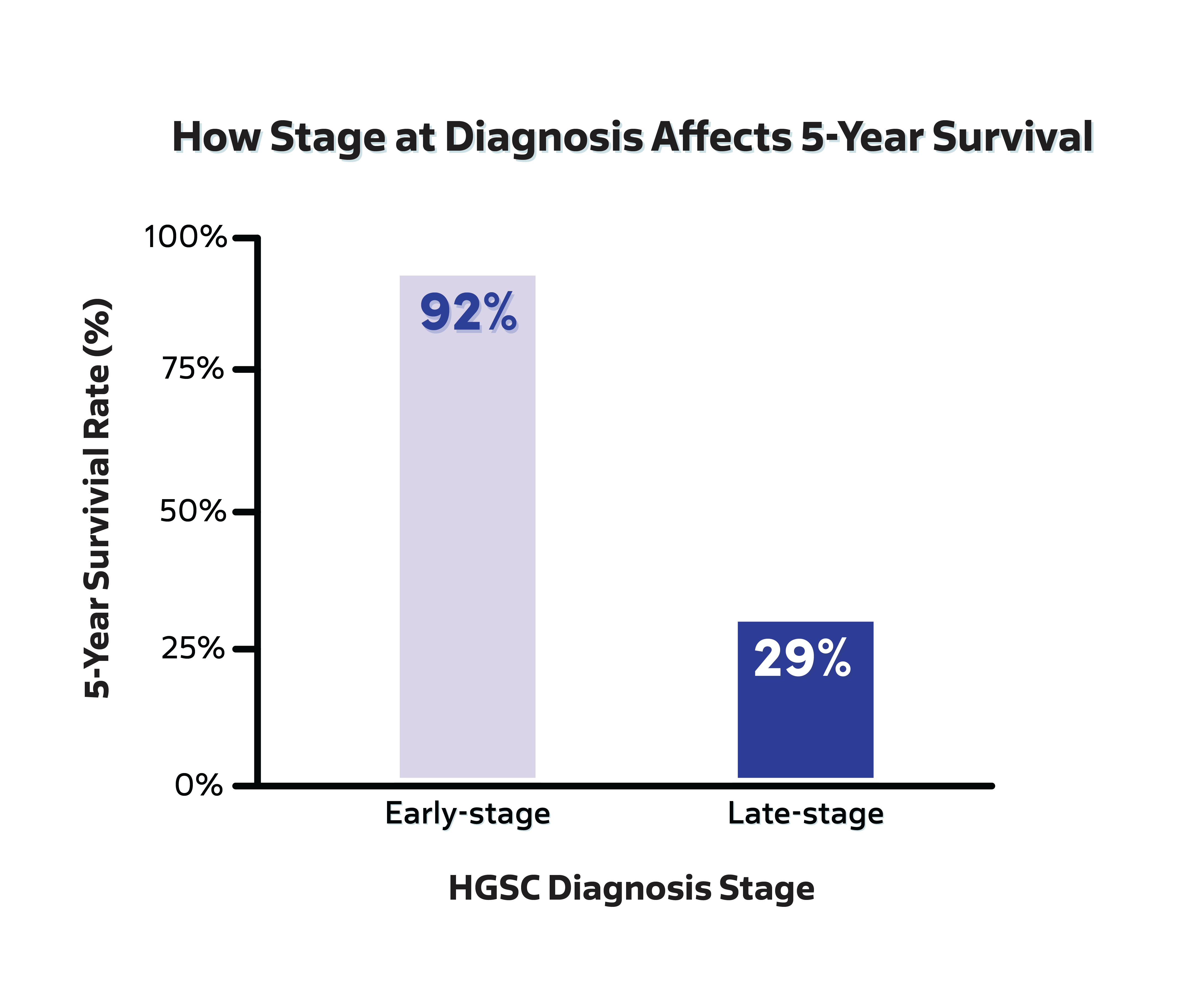
HGSC has a 5-year survival rate less than 50%
80% of patients diagnosed with HGSC have no known familial or genetic risk
Expanding access to salpingectomy can save lives
Universal adoption of bilateral salpingectomy in place of tubal ligation—and at the time of hysterectomy—provides a critical opportunity to reduce the risk of ovarian cancer. Expansion to other abdominal surgeries, such as appendectomy (removal of the appendix), cholecystectomy (removal of the gall bladder), hernia repair, cystectomy (removal of all or part of the urinary bladder), and colon resection is on the horizon.
Professional recommendations echo this discovery
Professional organizations around the world support bilateral salpingectomy instead of a tubal ligation (tying the tubes). They also recommend that patients consider salpingectomy when having an abdominal surgery (for example: ovarian cyst removal) and want to reduce their risk of ovarian cancer and permanently prevent pregnancy.
Royal College of Obstetricians and Gynaecologists
Women who are not at high risk for BRCA mutation and have completed their families should be carefully considered for prophylactic removal of the fallopian tubes with conservation of the ovaries at the time of gynaecological or other intraperitoneal surgery.
American College of Obstetricians and Gynecologists (ACOG)
The surgeon and patient should discuss the potential benefits of the removal of the fallopian tubes during a hysterectomy in women at population risk of ovarian cancer who are not having an oophorectomy. Prophylactic salpingectomy may offer clinicians the opportunity to prevent ovarian cancer in their patients.
Committee on Gynecologic Practice (Committee within ACOG)
Current attempts at screening for ovarian cancer have been unsuccessful and are associated with false positive test results that lead to unnecessary surgery and clinical complications. Prophylactic salpingectomy may offer clinicians the opportunity to prevent ovarian cancer in their patients.
Society of Gynecologic Oncology
For women at average* risk of ovarian cancer, risk-reducing salpingectomy should also be discussed and considered with patients at the time of abdominal or pelvic surgery, hysterectomy, or in lieu of tubal ligation.
*Average risk: no known hereditary risk of ovarian cancer.
Provincial Health Services Authority
Salpingectomy for average risk* women: For women who are undergoing any pelvic surgery and who have met their reproductive needs, consideration should be given to removal of the fallopian tubes.
*Average risk: no known hereditary risk of ovarian cancer.
Royal Australian and New Zealand College of Obstetricians and Gynaecologists
Doctors should discuss the risks and benefits of bilateral salpingectomy with patients undergoing hysterectomy for benign disease.
Kommission Ovar of the AGO
During preoperative counseling prior to hysterectomy, all patients should be informed about the potential beneficial impact of salpingectomy and the associated risk.
The International Federation of Gynecology and Obstetrics (FIGO)
FIGO recognizes the urgent need for safe and effective preventive measures against epithelial ovarian cancer—one of the most lethal gynecological malignancies—and supports bilateral salpingectomy as a standard care practice for women undergoing abdominal or pelvic surgery who have completed their families.
Acceptability to Providers and Patients
A recent survey from the American College of Obstetricians and Gynecologists found that 77% of gynecologists offer their patients bilateral salpingectomy at the time of hysterectomy to help lower their risk of ovarian cancer.
Patient-centered outcomes research shows that the majority of patients would choose bilateral salpingectomy at the time of another planned abdominal surgery.

We have more work to do
Recent research has shown that not all groups of women have equal access to bilateral salpingectomy. Outdated health policy is one major barrier. Thus, there is still a lot of work to do to make sure all women have equal access to salpingectomy as an important cancer prevention option in order to reduce ovarian cancer cases across all communities.
As of right now, salpingectomy at the time of non-gynecologic surgeries is not available to most people. Fixing this gap will require dedicated collaboration between different types of doctors and surgeons.
Ensuring all people know about and are able to choose salpingectomy to reduce their risk of ovarian cancer if and when the time is right for them is a main purpose of this online resource.

We are all in
The Outsmart Ovarian Cancer Collaborative (OOCC) is a renowned team of experts from four of the premier academic cancer centers in the US. We are conducting ongoing research and building awareness until a future free of ovarian cancer becomes a reality.
The Collaborative’s Mission is: to significantly decrease ovarian cancer incidence and deaths by ensuring that prevention becomes a standard of care that is known and accessible to all through education, advocacy, and innovation.
Their Vision is: a world where ovarian cancer is no longer a major threat because prevention is a standard of care that all know about and are empowered to choose.